Researchers have shown that patients fitted with a chip in their eye are able to integrate what the chip “sees” with objects their natural peripheral vision detects.
Two years ago, the researchers showed that with a thin, pixelated chip and specially designed glasses, they could restore limited vision in the center of the visual field of patients suffering from macular degeneration.
Now, in a follow-up study, they found that this prosthetic vision naturally integrated with the patients’ peripheral vision, which was unaffected by the disease.
The patients could simultaneously identify the orientations of colored lines in the center and sides of their visual field. The results suggest that the treatment could be used to restore functional vision.
That the patients were able to see a coherent image “is very exciting news,” says study lead author Daniel Palanker, professor of ophthalmology at Stanford University, because all previous retinal implants created “very distorted” perception.
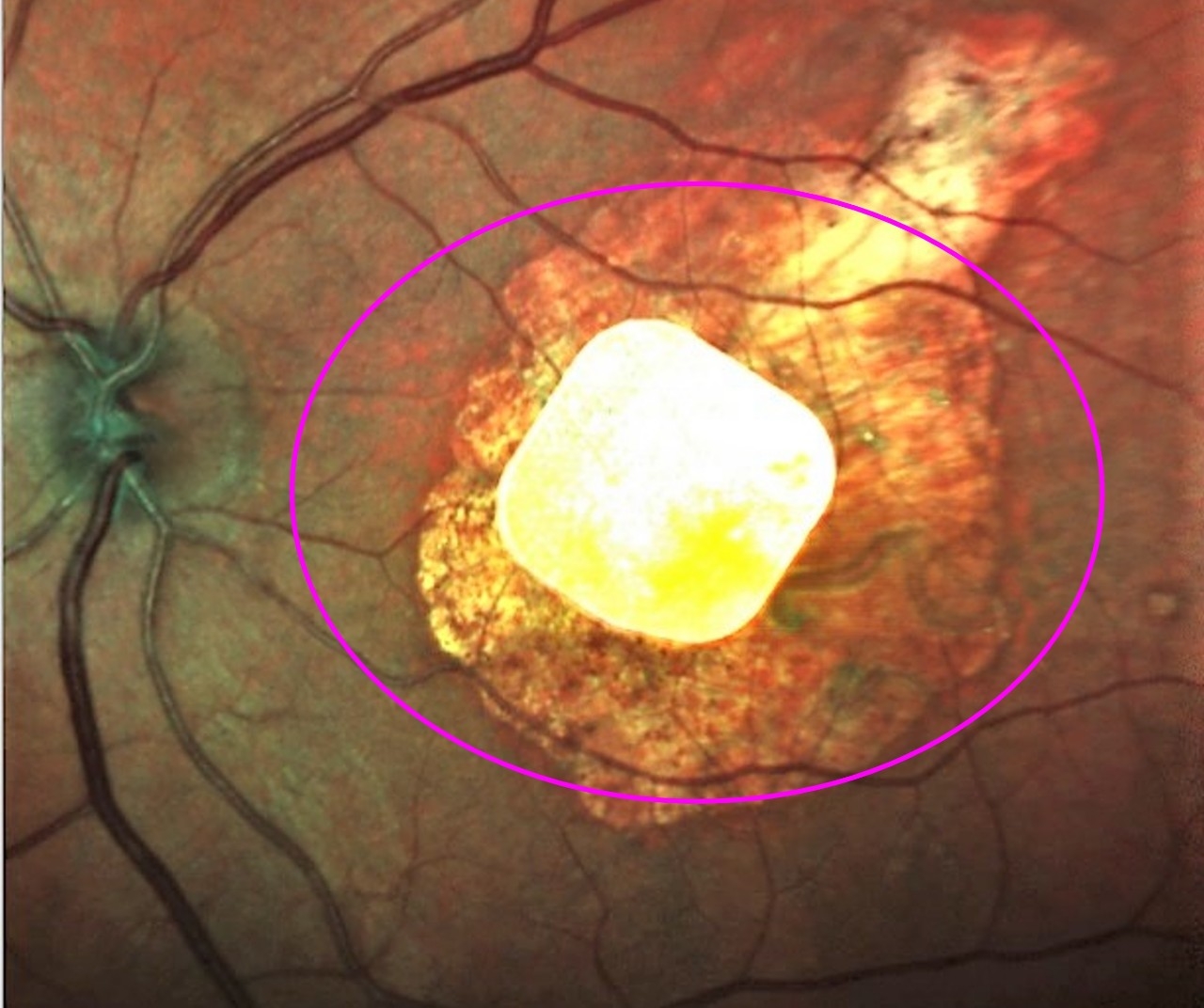
Macular degeneration, which affects 200 million people worldwide, most of whom are over 60 years old, causes patients to gradually lose sight in the center of their visual field. It’s debilitating because the remaining peripheral vision has low resolution. These patients have difficulty reading, recognizing faces, and performing other tasks of daily living.
The condition occurs when the photoreceptor cells in the center of the retina, known as the macula, degenerate. These tightly packed cells, which line the back of the eye, sense light and send signals to other retinal neurons, which transfer them to the brain, allowing visual perception. When photoreceptor cells degrade, the brain no longer receives the information it needs to create a detailed and coherent picture.
Current treatments for macular degeneration—such as vitamins and drugs targeting blood vessels that invade the macula and block vision—can slow the visual decline. But they can’t stop the degeneration or restore sight once the photoreceptors are gone.
Sensing light and seeing patterns
Nearly two decades ago, Palanker had the idea of creating a retinal prosthesis that would replace photoreceptor cells and take over their role of the light relay, as long as the nerve cells that the photoreceptors talk to were intact. (Inner retinal neurons can be destroyed by other visual disorders, such as glaucoma.)
The first step was to develop a thin device that could convert light into electric currents and that surgeons could implant into the back of the eye. The 1/12-inch pixelated chip sends electrical signals through the retinal neural network to the brain, restoring perception in the center of the visual field. The team also developed glasses equipped with a video camera that transmits images to the chip. A near-infrared display on these glasses beams the intensified video stream to the chip in the back of the eye.
“We are replacing lost photoreceptors in age-related macular degeneration with photovoltaic pixels,” Palanker says. “And we activate them with invisible light projected from the augmented reality glasses.”
After extensive preclinical research, Palanker’s collaborators in France recruited five patients, all over 60, who had advanced macular degeneration with no photoreceptors left in the central macula.
The patients retained the inner retinal nerve cells that could receive signals from the implant. Surgeons detached the retina above the blind spot, slid the chip underneath, and reattached the retina over it. The procedure lasted about two hours.
A few months after the surgery, the team found that with the help of the implant, patients could sense light and see patterns projected from the camera onto their retinas, such as lines and letters. Palanker and his team published the results of that in February of 2020.
‘Better than expected’ results
But two questions remained for a follow-up study. The first: Would patients be able to integrate their prosthetic central visual perception with the remaining natural peripheral vision? The initial tests were conducted with the virtual reality glasses: They explored only whether patients could see the projected lines and letters, while the peripheral natural vision was blocked. The second: Would this prosthetic vision last?
According to the new study, the answer to both of those questions is yes.
In the initial study, one patient’s chip was implanted incorrectly, and one patient later died of causes unrelated to the implant.
In the follow-up, not only were the three remaining patients able to see images projected onto the implant, but they could simultaneously use their peripheral vision. The researchers showed the patients pictures of two lines—one projected directly onto the implant with invisible near-infrared light, the other, displayed on a screen farther away. The latter forced them to use their natural peripheral vision. Each line was of a different color, and scientists asked patients what the orientations of each line was.
The patients had “no trouble properly seeing both patterns at once,” says Palanker, “indicating that the brain can perceive the prosthetic and natural retinal codes simultaneously.” The results were “even better than we expected.”
Currently, the prosthetic visual acuity is limited to about 20/460, which allows the patients to see large letters. “This is an exciting proof of concept,” Palanker says. “However, to make it a really useful device and applicable to many patients, we need to improve resolution.”
His team is working on an implant with much smaller pixels, which already matched the natural visual resolution in rats. He hopes that the new chip will provide better visual acuity for patients, potentially exceeding 20/100. Future studies will also test the implants in more natural settings, like the home, with more patients and for longer periods of time.
The paper appears in .
Pixium Vision, the Sight Again project, Inserm-DGOS, LabEx LIFESENSES, IHU FOReSIGHT, the National Institutes of Health, and Research to Prevent Blindness funded the work.
Source: Emma Yasinski for



